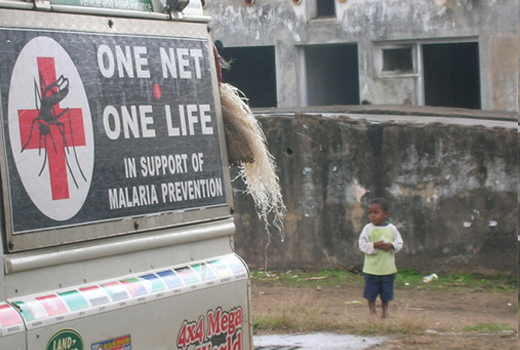
U.S. Navy Medicine: Fighting the War Against Malaria
The U.S. Department of Defense (DoD) sponsors substantial malaria research worldwide. Malaria is not a unique military infectious disease, it is a major global health issue and, according to the World Health Organization (WHO) World Malaria Report, 216 million cases and an estimated 655,000 deaths occurred in 2010. Most deaths occur among children living in Africa where a child dies every minute from malaria, and the disease is responsible for approximately 22 percent of all childhood deaths. As such, malaria infections are a tremendous burden for economic development and public health care systems in endemic countries. According to WHO, malaria can decrease gross domestic product (GDP) by as much as 1.3 percent in countries with high transmission levels. Long term, these aggregated annual losses have resulted in substantial differences in GDP between countries with and without malaria, particularly in Africa. Health costs of malaria include both personal and public expenditures on prevention and treatment. In some heavy-burden countries, the disease accounts for up to 40 percent of public health expenditures, 30 to 50 percent of inpatient hospital admissions and up to 60 percent of outpatient health clinical visits. Malaria disproportionately affects poor people who cannot afford treatment or who have limited health care access, trapping families and communities in a downward spiral of poverty.
Malaria has had a significant impact on U.S. military operations throughout history. It was responsible for a greater loss of manpower than enemy fire in all conflicts occurring in tropical regions during the 20th Century. And, it continues to present a major challenge to force health protection during operations in any environment where malaria is endemic. This includes 108 countries spanning the tropical and subtropical regions of the world, including most of sub-Saharan Africa and large regions of South Asia, Southeast Asia, Oceania, central Asia, the Middle East, Central and South America and the Caribbean. In a malaria-naïve military population, an infection can severely degrade performance, result in missed duty and may lead to prolonged hospitalization, and, in some cases, death.
Despite available malaria drug prophylaxis and personal protective measures, it remains one of the most significant potential mission-aborting disease non-battle injury (DNBI) threats to U.S. military personnel deployed to tropical regions of the world. Malaria transmission is year-round in Liberia, and a military mission was seriously altered there in 2003 when 43 deployed Marines were evacuated because of the disease. Five of the Marines required intensive care before recovering. And, in 2009 a Seabee deployed to this West African country died of malaria. Navy Medicine researchers, along with other partners, are working with the Liberian Institute for Biomedical Research and the U.S. Centers for Diseases Control to develop the country’s laboratory capability and mosquito surveillance program.
Disease Transmission

Photo by Nathan Miller, USAID/Benin|African Insecticide Residential Spray Campaign operator spraying house walls for malaria.
Malaria is transmitted through the bites of female Anopheles mosquitoes. In many places, transmission is seasonal with the peak during and just after the rainy season. The rate of transmission depends on factors related to the parasite, mosquito, human host and environment. Malaria is a complex parasite and requires a human host to live. The parasite lives part of its multistage life in mosquitoes and its later stages in humans. The mosquito transmits the microscopic parasites when it bites a human to extract blood for feeding. The parasite takes on different forms as it travels through the host’s body and eventually attacks the hemoglobin in the red blood cells.
If one single malaria parasite enters an individual’s blood stream after the bite of an infected mosquito and invades a liver cell, the parasite multiplies in five days to produce 30,000 to 40,000 progeny parasites, which are released into the blood when the liver cell ruptures. In the blood, each parasite invades a red blood cell and grows within 48 hours to produce 8 to 24 copies of itself, which are released back into the blood when red blood cells rupture. Within one or two weeks, these replicating parasites lead to as many as one trillion circulating in the blood stream. People who get malaria are typically very sick with high fevers, shaking chills and flu-like illness; the disease can cause coma and death.
Although malaria can be a deadly disease, severe illness and death can be prevented if protective measures are taken. Very effective drugs are available to treat individuals suffering from malaria, but the most cost-effective measure to fight this disease is to develop preventive malaria vaccines. Vaccines offer a “fire and forget” preventive strategy that provides much less burden to deployed military personnel than current prevention methods, which consist of drug prophylaxis and use of insecticides and repellants to deter the mosquito. It is not easy to develop a vaccine for malaria. Unlike other pathogens, like the polio virus for example, the malaria parasite constantly changes its immune makeup and has so far resisted scientists’ attempts to create a suitable vaccine treatment.
Navy Vaccine Program
The Navy’s Malaria Vaccine Program is located at the Naval Medical Research Center in Silver Spring, Md. The program’s strategy is based on the idea that protective immunity will depend on using multiple antigens to induce both cellular and humoral immunity. Researchers are using genomic and proteomic strategies to identify novel proteins with potential as vaccine antigens. They are also investigating the protective potential of attenuated malaria parasites.
Navy Medicine researchers are designing gene-based vaccines to interrupt the destructive life cycle in the early liver stages of infection before the damaging blood stages even start. The current gene-based vaccine combines two adenovirus vectors, each containing the gene for a different malaria protein. The adenovirus vectors are designed to carry the malaria gene (DNA) into the muscle cells of the body where the malaria genes are used as templates to express the malaria proteins, which in turn induces a strong immune response. The adenovirus-vectored gene-based approach induces killer T cells. These killer T cells detect the infected liver cells and destroy the cells as well as the parasite harbored within.
The next step for researchers will be to increase the number of malaria genes in the vaccine with the hope that adding genes will increase the level of protection to 80 percent or more of immunized volunteers from the current level of 27 percent. The goal is to develop a vaccine against malaria that protects 80 percent of vaccinated military personnel against infection for a minimum of six months.

U.S. Navy photo by Photographer’s Mate Airman Jordon R. Beesley | Hospital Corpsman 3rd Class Kevin Herbert
packs Doxycycline, a Malaria vaccination.
The program reached a new milestone in 2010 when researchers induced complete protection against malaria in four volunteers immunized with a novel gene-based candidate vaccine designed to prevent infection with the deadliest malaria parasite, Plasmodium falciparum. While more research needs to be done to further improve this novel vaccine, these initial results are very promising.
The program is conducting trials of candidate vaccines and successful vaccines can be transitioned to testing in field settings with collaborating institutions in Africa, Asia and South America. The Navy Malaria Program also benefits from the Navy’s and Army’s overseas laboratories, which allow study of the epidemiology of the parasite in its native habitat and also helps to coordinate field testing of novel vaccines.
Research Partners
In 2011 the Navy Malaria Program signed a cooperative research agreement with the Bill and Melinda Gates Foundation to promote development of malaria vaccines. In this three-year effort the laboratory will partner with the Army and Seattle BioMed, a non-profit research organization, to develop a systems biology approach to identify biomarkers of protection to guide vaccine development and deployment of vaccines in the field. In addition to conducting a clinical trial with a potential vaccine, they will also work on immunoassays and antigens.
Navy Medicine researchers are actively engaged in capacity building in many countries. For example, since 1996 Navy Medicine has partnered with the West African nation of Ghana in designing and conducting public health research that measures the risk and impact of malaria. Researchers from the Naval Medical Research Center and the U.S. Naval Medical Research Unit No. 3 in Cairo, Egypt, along with their colleagues at the Noguchi Memorial Institute for Medical Research in Accra, Ghana, and the Ghana Ministry of Health, have worked together to develop ways to control, prevent and treat malaria. The program has expanded to include more laboratories in Ghana and the Center for Malaria Research in Ouagadougou, the capital of the neighboring country of Burkina Faso.
The U.S. Navy-Ghana collaboration was instrumental in winning a five-year malaria research grant from the U.S. National Institute of Allergies and Infectious Disease for 2001 to 2006 and was successful in a grant renewal for 2006 to 2011. In 2010 the main clinical laboratories in Ghana and Burkina Faso initiated two early phase malaria vaccine trials performed by Africans for Africans. Throughout the last five years, focus of the joint research has broadened beyond malaria to include outbreak investigations and cross-training in field and laboratory methods for the study of leishmaniasis, influenza, Lassa fever and rotavirus, and it continues to connect the nations in scientific productivity.
Researchers from the U.S. Naval Medical Research Unit No. 6 in Lima, Peru, joined a consortium of institutions from Peru, Brazil and the U.S. to develop a Center of Excellence for malaria research that will work towards control and eventual eradiation of malaria from the Amazon region. The Center of Excellence is supported by a multi-year grant from the U.S. National Institutes of Health. Ongoing field and laboratory efforts are determining malaria incidence rates, genotyping parasites, monitoring drug resistance and determining which mosquitoes are transmitting malaria in the areas. The Center is developing a new generation of international malaria researchers.
Enduring friendships and trust can be built by working together with other countries to monitor, prevent and treat malaria and other infectious disease threats.